Preventative Sensor-Based Remote Monitoring of the Diabetic Foot in Clinical Practice

Published in Sensors, leading international, peer-reviewed, open access journal on the science and technology of sensors.
Evan Minty1 MD MSc, Emily Bray2 MBA, Courtney B. Bachus2 MBT, J. Breanne Everett2 MD MBA, Karen M. Smith2 BSc, David G. Armstrong3 DPM MD PhD, Brock Liden4 DPM
1 Faculty of Medicine, University of Calgary, Canada
2 Orpyx Medical Technologies, Inc., Canada
3 Keck School of Medicine, University of Southern California
4 Cutting Edge Research, Ohio
Abstract
Diabetes and its complications, particularly diabetic foot ulcers (DFUs), pose significant challenges to healthcare systems worldwide. DFUs result in severe consequences such as amputation, increased mortality rates, reduced mobility, and substantial healthcare costs. The majority of DFUs are preventable and treatable through early detection. Sensor-based remote patient monitoring (RPM) has been proposed as a possible solution to overcome limitations, and enhance the effectiveness, of existing foot care best practices. However, there are limited frameworks available on how to approach and act on data collected through sensor-based RPM in DFU prevention. This perspective article offers insights from deploying sensor-based RPM through digital DFU prevention regimens. We summarize the data domains and technical architecture that characterize existing commercially available solutions. We then highlight key elements for effective RPM integration based on these new data domains, including appropriate patient selection and the need for detailed clinical assessments to contextualize sensor data. Guidance on establishing escalation pathways for remotely monitored at-risk patients and the importance of predictive system management is provided. DFU prevention RPM should be integrated into a comprehensive disease management strategy to mitigate foot health concerns, reduce activity-associated risks, and thereby seek to be synergistic with other components of diabetes disease management. This integrated approach has the potential to enhance disease management in diabetes, positively impacting foot health and the healthspan of patients living with diabetes.
Summary
- By addressing foot health concerns proactively and promoting active lifestyles, sensor-based RPM can positively impact not only foot health but also the overall disease trajectory and healthspan of people living with diabetes.
- Sensor-based RPM programs can help address the limitations of traditional diabetic foot care by identifying pre-ulcerative conditions before they progress to more serious complications.
- A practical framework for integrating RPM into clinical practice and DFU prevention regimens has been developed based on the authors' experiences with sensor-based RPM.
- Recommended actions for clinicians after a patient has been escalated from remote care to in-office care are provided.
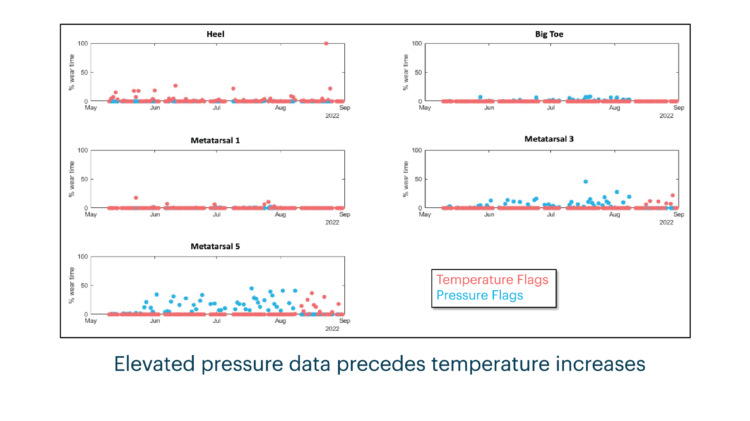
- DFU complications are influenced by various factors, making it essential to assess physiological and behavioral data from multiple domains such as pressure, temperature, and activity.
- Sensor-based RPM allows clinicians to intervene at different stages of the disease process, gain insights into disease pathogenesis, and improve predictive models for DFU.
- RPM for diabetic foot care should be part of a comprehensive disease management approach, aligned with other diabetes care principles to optimize glycemic control and reduce cardiovascular risk. It should include activity monitoring, prescription, modulation, and motivational interviewing based on sensor-derived physiological data.
Evaluating the Effectiveness of Plantar Sensory Insoles and Remote Patient Monitoring for Early Intervention in Diabetic Foot Ulcer Prevention in Patients with Peripheral Neuropathy
Innovative Plantar Sensory Insoles To Prevent Foot Ulcer Recurrence and Guide Treatment Plans in Patients With Diabetic Peripheral Neuropathy
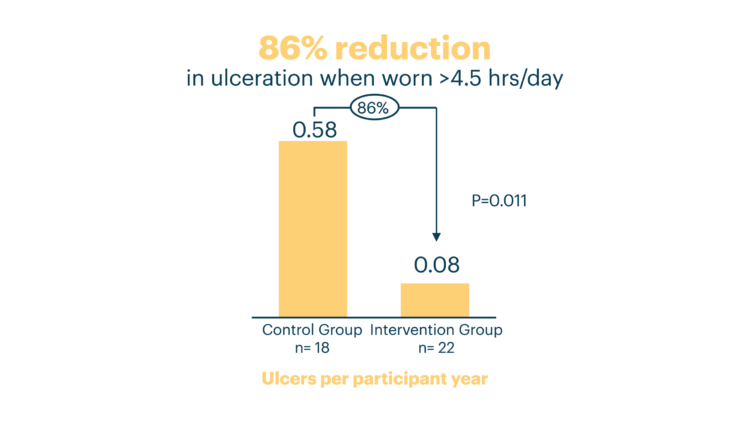
Innovative Intelligent Insole System Reduces Diabetic Foot Ulcer Recurrence at Plantar Sites: A Prospective, Randomized, Proof-of-Concept Study