The Orpyx Sensory Insole Program
Backed by a Robust and Growing Body of Evidence

Committed to Research
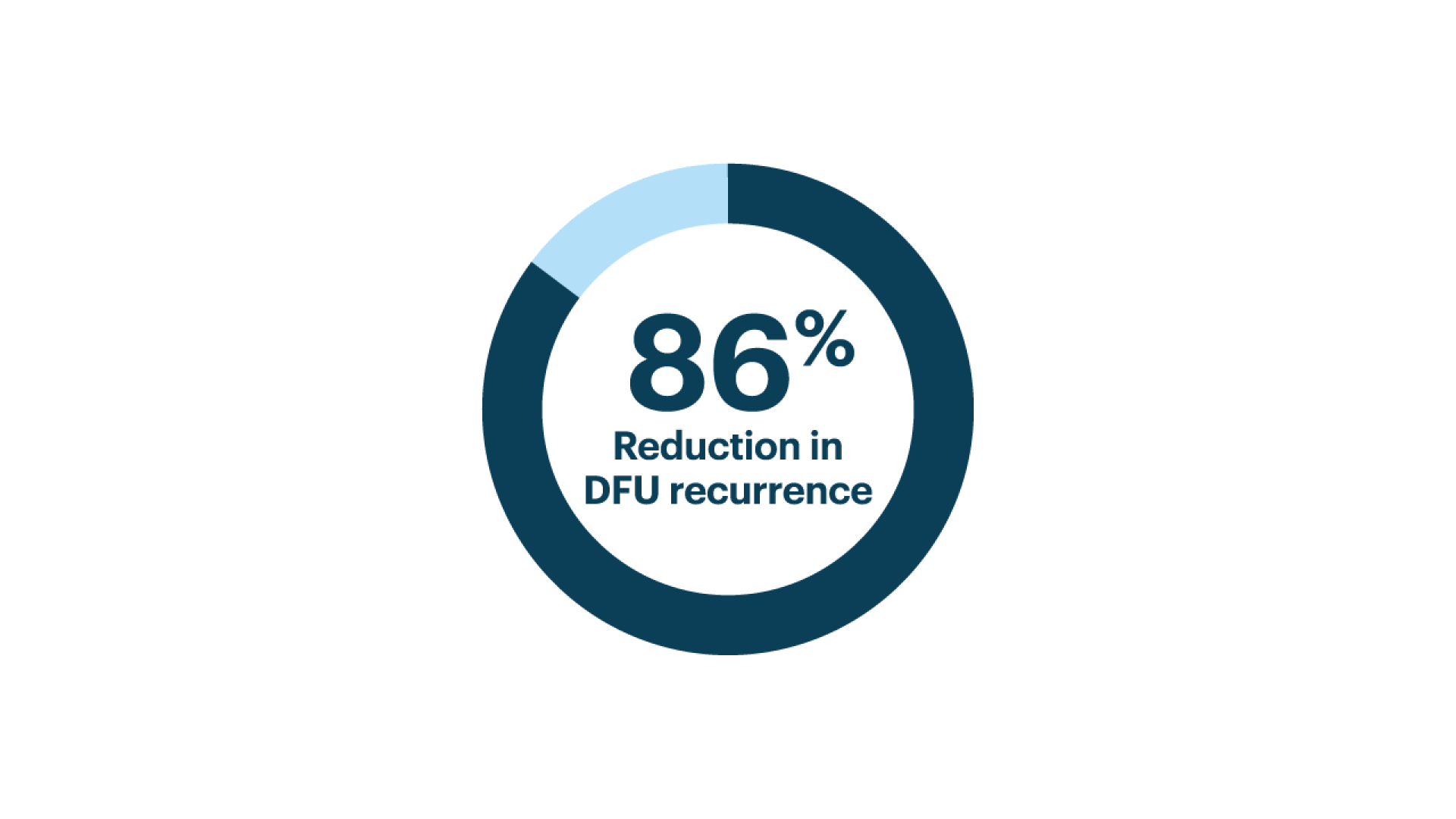
The Only Plantar RPM Solution Backed by a Randomized Controlled Trial¹
In a randomized controlled trial of patients with diabetes and a history of foot ulcers, the Orpyx technology, delivering real-time pressure alerts, demonstrated a substantial reduction in ulcer recurrence.
Among patients who wore the insoles for at least 4.5 hours per day, ulcer incidence was reduced by 86% compared to standard care.¹
This highlights the critical role of consistent use and real-time data in supporting early intervention and long-term limb preservation.
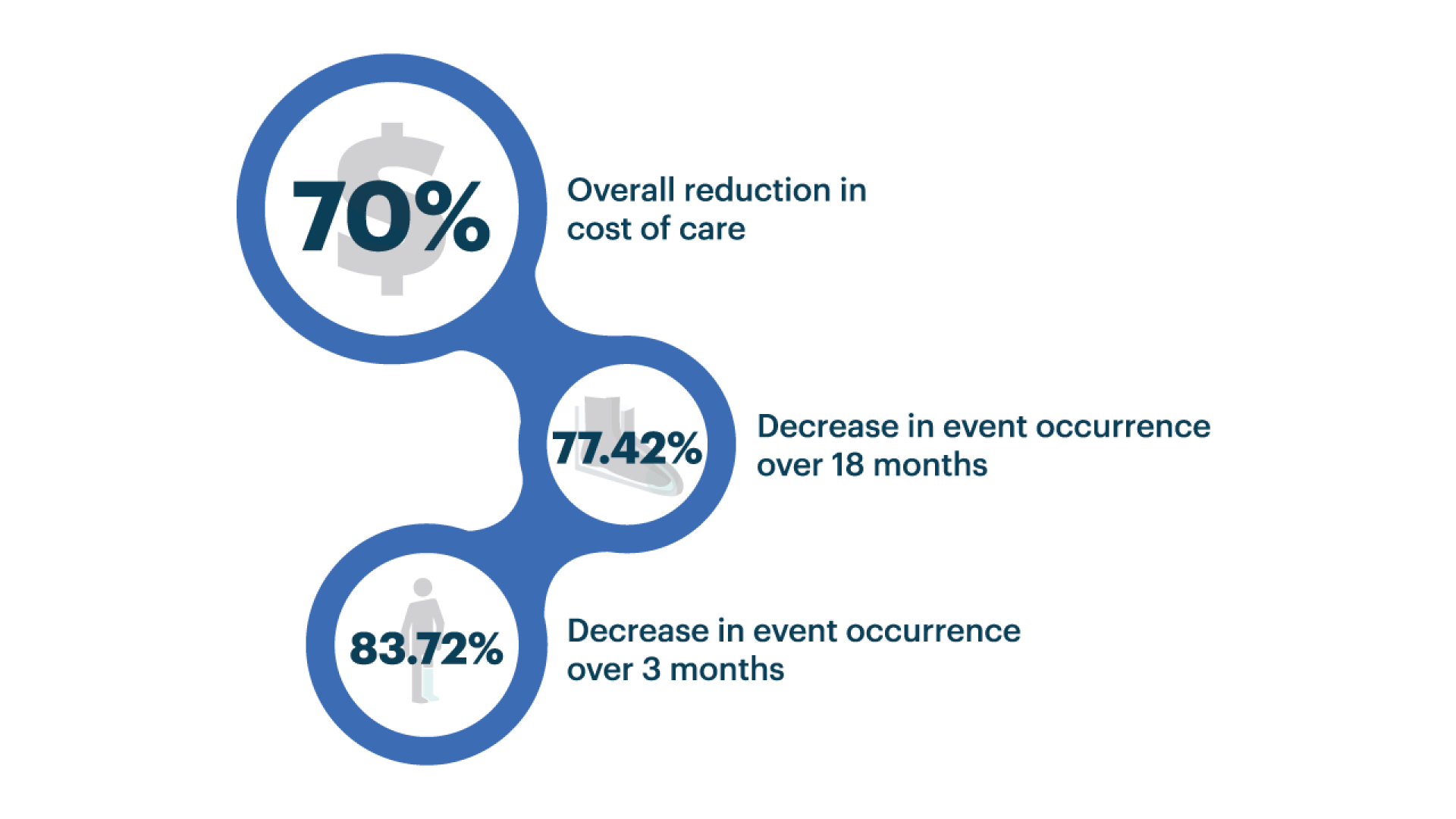
Significant Reduction in Foot Ulcer Occurrence and Healthcare Costs with SOC + Orpyx Technology²
This cost-effectiveness study evaluated standard of care (SOC) alone versus SOC combined with the Orpyx technology. Cost analysis was conducted over both short-term (3 months) and long-term (18 months) periods to assess clinical and economic outcomes.
The peer-reviewed study demonstrated sustained prevention benefits over 18 months, with substantial healthcare cost savings and a significant reduction in event occurrences.2
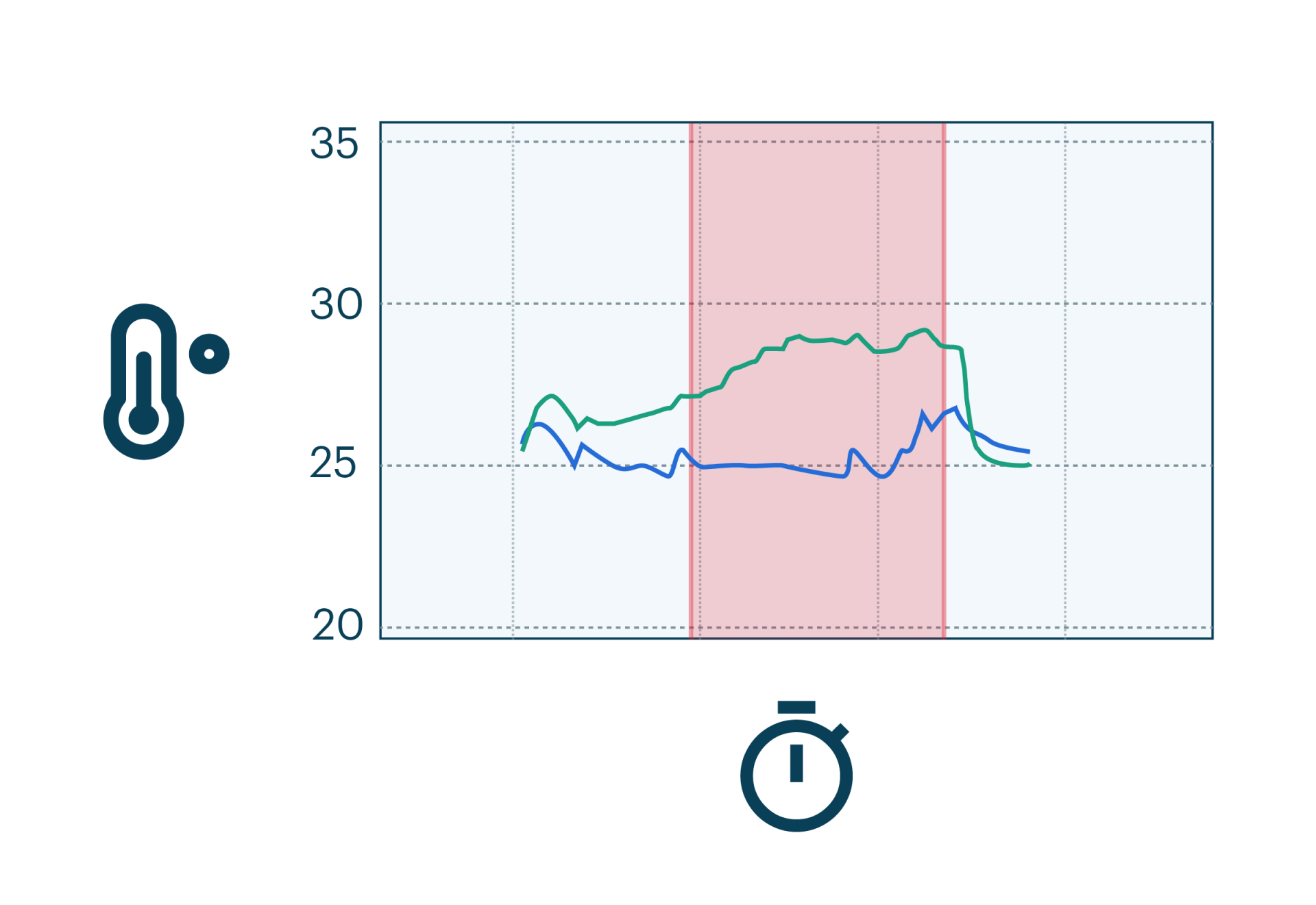
Exploring the Value of Continuous Plantar Temperature Monitoring for Diabetic Foot Health Management: Observations from a Prospective Study
There is increasing evidence that plantar temperature monitoring can reduce the incidence and recurrence of DFUs. While daily monitoring has been shown to help detect early signs of inflammation, by continuously tracking intra-day temperature asymmetries with the Orpyx Sensory Insoles, this research reveals that plantar temperature signals often fluctuate significantly throughout the day.
These findings suggest that single daily readings may be insufficient to reliably capture meaningful changes, potentially leading to missed warning signs or false alarms.
Clinical Research
Orpyx Clinical Research
- Innovative intelligent insole system reduces diabetic foot ulcer recurrence at plantar sites: a prospective, randomised, proof-of-concept study. Abbott et al (2019)
- Cost effectiveness of smart insoles in preventing ulcer recurrence for people in diabetic foot remission. Najafi et al (2018)
- Smarter Sole Survival: Will Neuropathic Patients at High Risk for Ulceration Use a Smart Insole-Based Foot Protection System? Najafi et al (2017)
- A Foreign Body Through the Shoe of a Person with Diabetic Peripheral Neuropathy Alters Contralateral Biomechanics. Chatwin et al (2018)
- Use of the SurroSense Rx System for Sensory Substitution of the Insensate Plantar Aspect Resurfaced with Latissimus Dorsi Muscle Free Flap and Skin Graft: A Retrospective Case Study. Bray et al (2017)
- Novel Pressure-Sensing Smart Insole System Used for the Prevention of Pressure Ulceration in the Insensate Foot: A Case Report. Alfonso & Chiu (2017)
- Validation of Plantar Pressure Measurements for a Novel In-Shoe Plantar Sensory Replacement Unit. Ferber et al (2013)
Plantar Pressure
- The Role of Pressure Offloading on Diabetic Foot Ulcer Healing and Prevention of Recurrence. Bus S. (2016)
- In-shoe pressure thresholds for people with diabetes and neuropathy at risk of ulceration: a systematic review. Jones et al (2021)
- The role of foot pressure measurement in the prediction and prevention of diabetic foot ulceration – a comprehensive review. Chatwin et al. (2019)
- Measuring Plantar Tissue Stress in People With Diabetic Peripheral Neuropathy: A Critical Concept in Diabetic Foot Management. Lazzarini et al (2019)
- Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Waaijman et al (2014)
Thermometry
- Efficacy of at home monitoring of foot temperature for risk reduction of diabetes-related foot ulcer: A meta-analysis. Golledge et al (2022)
- Home Monitoring of foot skin temperatures to prevent ulceration. Lavery et al (2004)
- Preventing diabetic foot ulcer recurrence in high-risk patients: Use of temperature monitoring as a self-assessment tool. Lavery et al (2007)
- Skin temperature monitoring reduces the risk for DFU in high-risk patients. Armstrong et al (2007)
Step Count and Activity
- Variability in activity may precede diabetic foot ulceration. Armstrong et al (2004)
- Comparison of physical activity and cumulative plantar tissue stress among subjects with and without diabetes mellitus and a history of recurrent plantar ulcers. Maluf & Mueller (2003)
- Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Colberg et al (2016)
DFU Clinical Guidelines
1. Abbot CA, et al. Innovative intelligent insole system reduces diabetic foot ulcer recurrence at plantar sites: a prospective, randomised, proof-of-concept study. Lancet Digital Health Oct. 2019; 1: e308–18. (Study was conducted with first generation SurroSense Rx® which has the same pressure algorithm as the Orpyx technology) 2. Najafi B et al, Cost effectiveness of smart insoles in preventing ulcer recurrence for people in diabetic foot remission. Wound Care Management (2018) Volume 1(1): 5-7. 3. Data on file—Continuous_temperature_monitoring. *Study was conducted with first generation SurroSense Rx® which has the same pressure algorithm as Orpyx Sensory Insoles.